Inadequate support: There is no evidence that healthcare professionals are misdiagnosing flu cases as COVID-19 cases. COVID-19 cases are confirmed by PCR testing that is specific for SARS-CoV-2 and does not detect flu viruses. To be considered a probable COVID-19 case, several criteria, including previous contact with a COVID-19 case or a positive result in SARS-CoV-2 antigen or antibody testing, must also be met. A person would not be classified as a probable COVID-19 case based on symptoms alone.

AFFIRMATION COMPLETE: ”There is no evidence to support the contention that masks would stop influenza while failing to stop COVID”; “Influenza has been renamed COVID-19 in large part”
REVIEW
So far, the 2020-2021 flu season has seen fewer cases than in previous years, leading to allegations that flu cases are being misdiagnosed as COVID-19. These claims started circulating on social media in late 2020 and early 2021, including this article published by Just The News claiming that « influenza has been renamed COVID-19 in large part ». Health Feedback reviewed earlier posts claiming that flu was being diagnosed as COVID-19 and that “COVID-19 cured the flu” and found them to be misleading.
The article cites Knut Wittkowski, who formerly worked as a biostatistician at the Rockefeller University and who has spread COVID-19 misinformation in the recent past. Wittkowski’s previous defense of natural infection as the only way to achieve herd immunity against COVID-19 led the Rockefeller University to release a statement on 13 April 2020 saying that Wittkowski’s opinions « do not represent the views of the Rockefeller University, its leadership, or its faculty ».
No evidence that flu cases are being misdiagnosed as COVID-19
The U.S. Centers for Disease Control and Prevention (CDC) report COVID-19 cases and deaths through the COVID Data Tracker. Counts include all COVID-19 cases and deaths confirmed by PCR testing and, since 14 April 2020, probable COVID-19 cases and deaths. In some territories, probable cases and deaths aren’t confirmed by laboratory testing. COVID-19 PCR tests specifically detect the presence of genetic material from SARS-CoV-2, the virus that causes COVID-19, in a patient’s biological samples, such as mucus or saliva. As Health Feedback explained in a previous review, the COVID-19 PCR tests don’t detect other viruses, including the influenza viruses.
Wittkowski claims that probable COVID-19 cases may include « quite a number » of flu cases incorrectly diagnosed as COVID-19, since flu symptoms can be similar to mild COVID-19 symptoms. However, this reasoning is misleading, as it fails to acknowledge that a probable COVID-19 case or death is not classified as such based solely on symptoms, as the CDC explained in the 2020 Interim Case Definition:
« A probable case or death is defined by one of the following:
- Meeting clinical criteria AND epidemiologic evidence with no confirmatory laboratory testing performed for COVID-19
- Meeting presumptive laboratory evidence AND either clinical criteria OR epidemiologic evidence
- Meeting vital records criteria with no confirmatory laboratory testing performed for COVID19″
In addition, an incorrect diagnosis of flu cases as COVID-19 cannot explain the higher than usual mortality observed during the COVID-19 pandemic. Public health authorities monitor flu activity by collecting and analyzing epidemiological data throughout the entire year. Because relatively mild flu infections often go unreported, the CDC uses mathematical models to estimate the total number of flu illnesses, hospitalizations, and deaths during a flu season.
According to these estimates, flu accounted for 34,200 deaths in the 2018–2019 season and 61,000 deaths in the unusually severe 2017-2018 flu season. In contrast, at the time of this review’s publication, COVID-19 caused more than 387,000 deaths since the first reported death in February 2020, according to the CDC COVID Data Tracker. Therefore, even if all flu deaths in the U.S. were incorrectly attributed to COVID-19, they would account for less than 15% of the COVID-19 deaths reported so far across the country.
Face masks and other public health measures to reduce the spread of COVID-19 likely contributed to reducing flu transmission
The CDC has indeed reported lower flu activity across the U.S. than in previous years (see Figure 1). As of 2 January 2021, the weekly report on influenza surveillance noted:
« The percentage of visits to a health care provider for influenza-like illness (ILI) in week 53 is at 1.6% for the second week in a row. This is below the national baseline of 2.6%. ILI surveillance may be impacted by the COVID-19 pandemic and should be interpreted with caution ».
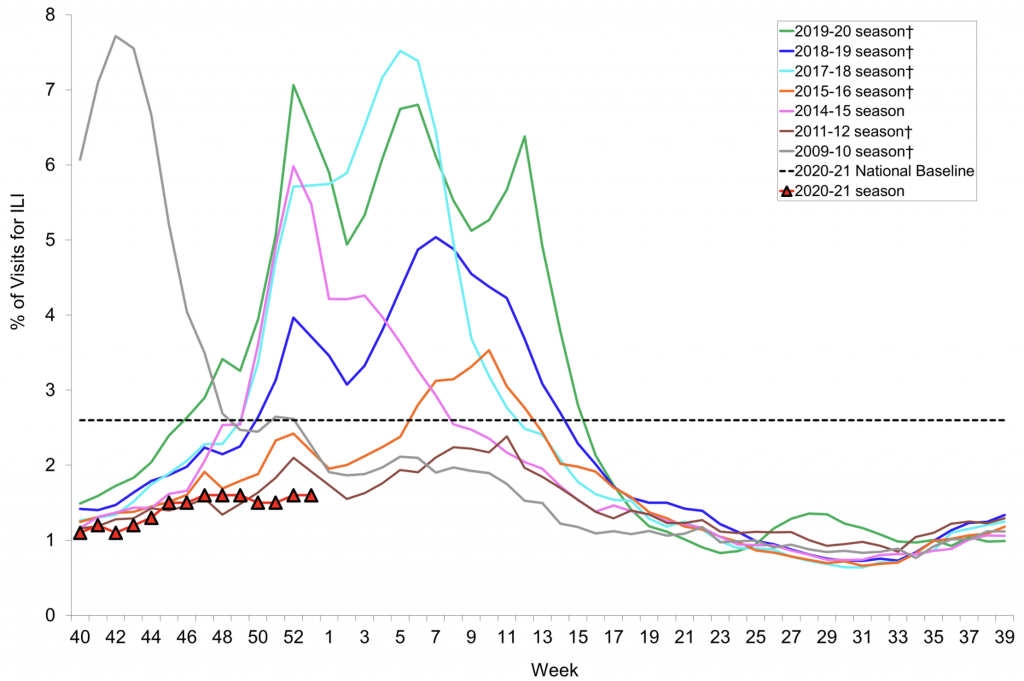
Figure 1. Percentage of visits for influenza-like illness (ILI), as reported by the U.S. outpatient Influenza-like Illness Surveillance Network (ILINet) for the 2020-2021 season and the past seven seasons. Source: Weekly U.S. Influenza Surveillance Report for Week 53, ending January 2, 2021. Note that data for the current 2020-2021 season (red line) is incomplete.
Likewise, weekly influenza updates from the World Health Organization (WHO) indicate a global decrease in flu activity for the current season:
« Globally, despite continued or even increased testing for influenza in some countries, influenza activity remained at lower levels than expected for this time of the year ».
While researchers have not determined the exact reasons for the decrease in flu activity this season yet, there is a general agreement that COVID-19 restrictions are likely contributing to the reduced flu activity. For example, a 2019 WHO document recommends that people wear face masks to reduce flu transmission:
« Face masks worn by asymptomatic people are conditionally recommended in severe epidemics or pandemics, to reduce transmission in the community. Although there is no evidence that this is effective in reducing transmission, there is mechanistic plausibility for the potential effectiveness of this measure. A disposable surgical mask is recommended to be worn at all times by symptomatic individuals when in contact with other individuals ».
Contrary to what the Just The News article claimed, research studies did not show that face masks can’t reduce flu transmission. Instead, the available evidence is insufficient to make definite conclusions regarding community mask use, as the WHO remarked on page 41:
« The evidence base on the effectiveness of NPIs in community settings is limited, and the overall quality of evidence was very low for most interventions. There have been a number of high quality randomized controlled trials (RCTs) demonstrating that personal protective measures such as hand hygiene and face masks have, at best, a small effect on influenza transmission, although higher compliance in a severe pandemic might improve effectiveness ».
Wearing face masks reduces the spread of COVID-19 by blocking the release of respiratory droplets from infected individuals. Therefore, wearing face masks likely reduces the transmission of other respiratory infections that spread in ways similar to COVID-19, including the flu. For this reason, Wittkowski claims that if face masks worked, then they should be able to stop both COVID-19 and flu equally. Several posts on Facebook and Instagram make similar allegations. As we explain below, such interpretations are misleading, as they overlook the fact that COVID-19 spreads easier than flu. Furthermore, other factors besides the use of face masks may also contribute to reducing flu transmission, such as an increase in flu vaccination rates.
In addition to the use of face masks, other public health measures to reduce the spread of COVID-19, such as physical distancing, frequent handwashing, and travel restrictions, can also limit the spread of other respiratory diseases. One indication that such measures effectively reduce the spread of flu is the sharp decrease in flu activity around March 2020, when many countries put in place restrictions to limit COVID-19 transmission. In addition, researchers observed a decline in most of the viruses that cause respiratory infections, except for rhinoviruses, which are the primary cause of the common cold.
According to health experts, increased flu vaccination is likely also contributing to the reductions in flu cases this season. As of 1 January 2021, the CDC’s Weekly National Vaccination Dashboard reported that 192.5 million doses of flu vaccine were distributed across the U.S., which is the highest number of doses distributed during a single flu season. During the Southern Hemisphere flu season, other countries showed record vaccination rates. For example, during the 2019-2020 season, Australia released 17.6 million doses of flu vaccine, which was 5 million more than the doses administered in the 2019-2020 flu season.
Although flu and COVID-19 are both contagious respiratory illnesses that can cause similar symptoms in infected individuals, they have significant differences that might affect transmission. First, COVID-19 involves more aerosol transmission and superspreading events than flu. Second, people infected with SARS-CoV-2 can take longer to develop symptoms than people who are infected with the flu, which increases the risk of presymptomatic transmission of COVID-19[1]. Finally, people infected with SARS-CoV-2 may be contagious for a longer period of time than those infected by flu viruses[2,3]. As a result, COVID-19 can spread more quickly and easily than flu, limiting the efficacy of public health measures.
In summary, no evidence supports the claim that flu cases are being misdiagnosed as COVID-19. Although both diseases share similar symptoms, probable COVID-19 cases must meet additional criteria besides the presence of disease symptoms, such as previous close contact with a COVID-19 case or a positive SARS-CoV-2 antigen or antibody test result. Social media posts questioning how public health measures can effectively limit the spread of flu but not COVID-19 are misleading as they fail to account for several factors, such as the differences in transmission between COVID-19 and flu. Experts suggest that the lower than usual flu activity this season is likely due to a combination of factors, including public health measures implemented to reduce the spread of COVID-19 and higher flu vaccination rates.
REFERENCES
- 1 – Wei et al. (2020) Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. Morbidity and Mortality Weekly Report.
- 2 – He et al. (2020) Temporal dynamics in viral shedding and transmissibility of COVID-19. Nature.
- 3 – Chun et al. (2020) Transmission onset distribution of COVID-19. International Journal of Infectious Diseases.



