
Misleading: An underlying assumption of the claim is that cloth masks are mainly intended to protect the wearer from infection. However, health authorities advise the public to use cloth masks to reduce the spread of COVID-19 from infected to uninfected people. Such masks are not intended to protect the wearer from infection.

RECLAMACION: “CDC study finds overwhelming majority of people getting coronavirus wore masks”; CDC study shows that more people who wear masks become sick with COVID-19 compared to non-mask wearers, therefore masks don’t work or are making us ill
REVIEW
Misinformation aimed at discouraging mask use has been prolific during the COVID-19 pandemic, as detailed in several reviews by Health Feedback. Claims that masks do not work or make people more likely to get COVID-19 began circulating and went viral on Facebook and other social media platforms like Twitter in early October 2020 (see example here). In addition to social media users, media outlets, including The Federalist, The Blaze, Fox News, and Breitbart, have also published similar claims. also published similar claims. These claims are allegedly supported by findings from a study published in September 2020 in the Mortality and Morbidity Weekly Report by the U.S. Centers for Disease Control and Prevention (CDC)[1].
The claim asserts the study found that people who wear masks become infected with the virus that causes COVID-19 more often than people who never wear a mask. Specifically, the claim cites figures from the study, which report that 3.9% of people who tested positive for COVID-19 reported never wearing a mask, whereas more than 80% reported wearing a mask either often or always (see table below).
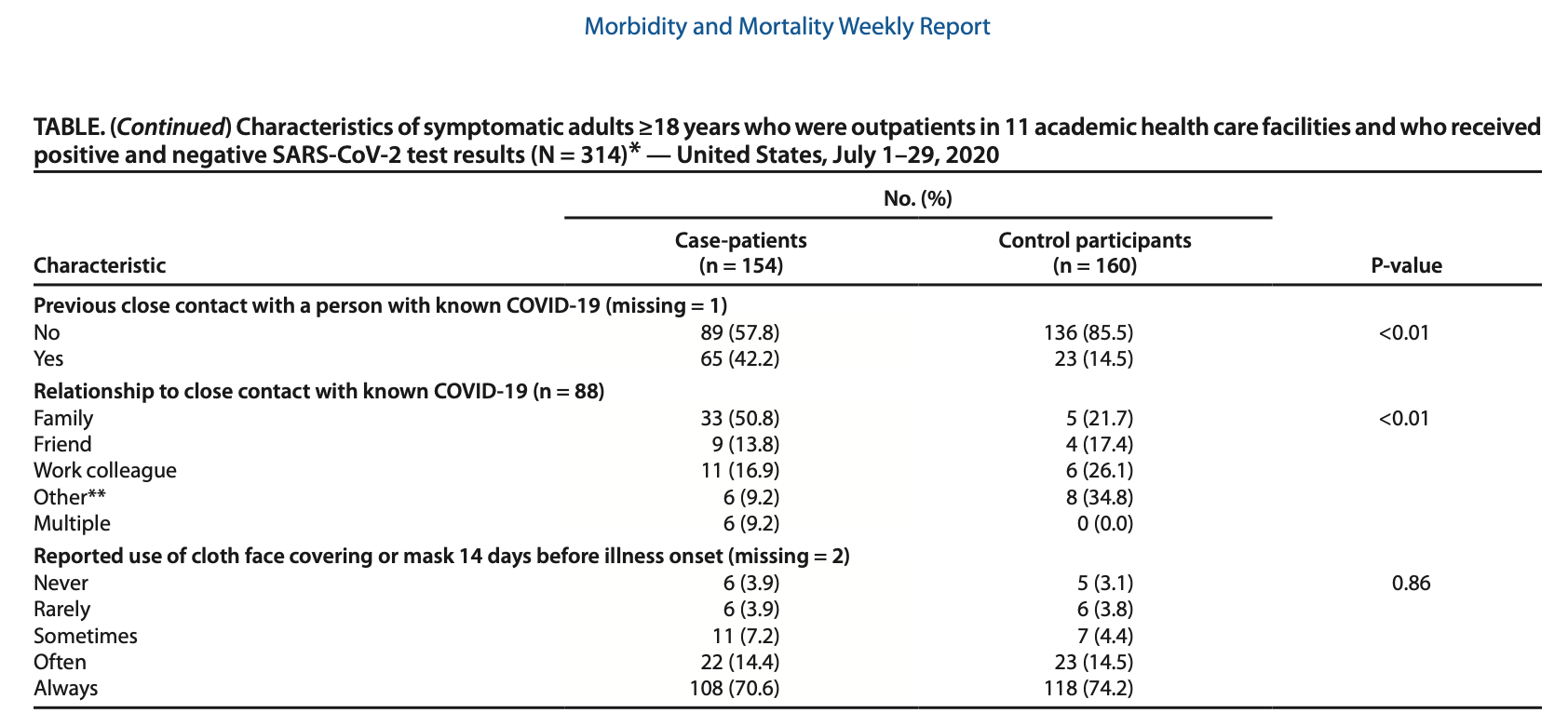
Table 1. The characteristics of people who tested positive for COVID-19 and those that tested negative. There were a total of 314 patients included in the study, 154 had tested positive for COVID-19 (case-patients), while 160 had tested negative for COVID-19 (control participants). Note that only 11 patients reported never wearing a mask, while 218 reported always wearing a mask.
Wesley Self, one of the study’s lead authors and associate professor at Vanderbilt University School of Medicine, told Health Feedback in an email, “We are not aware of any of our data showing that wearing a mask increases the risk for COVID-19.”
In response to the claim, the CDC clarified in an email to Health Feedback that:
“CDC guidance on masks has clearly stated that wearing a mask is intended to protect other people in case the mask wearer is infected. At no time has CDC guidance suggested that masks were intended to protect the wearers. [Editor’s note: CDC guidance has been updated.]
In studies like the MMWR published in September, it is difficult to detect the effect of an exposure or intervention when it is widely deployed or used. Both cases and controls in the study had high levels of mask use. They were likely achieving sufficient protection within their social network. However, in restaurants and other places where food and beverages are consumed, masks cannot be used.
Growing evidence increasingly shows that wearing masks in community settings reduces transmission among individuals in that community. There are laboratory studies, animal studies, community and epidemiological studies, as well as policy studies that show masking reduces transmission in communities by blocking exhaled respiratory droplets.”
The comparison made in the claim is highly flawed, as it fails to account for the fact that there were far more people who wear masks included in the study than people who do not. In fact, the study included a total of 314 individuals, among whom only 11 never wore masks. Considering that the people who wore masks greatly outnumber those who never wore masks, comparing the proportion of people who tested positive for COVID-19 between the two groups would show mask wearers to be the majority by default. In other words, this comparison simply demonstrates the vast differences in group size of the people included in the study. It is not evidence that masks make people ill or do not work, contrary to the assertions or implications made in some posts and articles.
Another problem with the comparison is that the population surveyed in the study may not accurately represent the general U.S. population or all COVID-19 patients (sampling bias). As a result, the findings of the study may not be generalizable to the rest of the population. It is therefore inaccurate and misleading to claim, as some have, that the study shows that people who wear masks make up the majority of COVID-19 cases. As the authors pointed out in their study:
“[T]he sample included 314 symptomatic patients who actively sought testing during July 1–29, 2020 at 11 health care facilities. […] Persons who did not respond, or refused to participate, could be systematically different from those who were interviewed for this investigation.”
The study explored how close contact with people diagnosed with COVID-19, as well as different types of community activities, including shopping, going to the gym, and going to restaurants, are associated with different likelihoods of infection. The study surveyed adults who developed signs and symptoms consistent with COVID-19 and who were tested at outpatient clinics by telephone. Patients were asked to report whether they had participated in various community activities during the 14 days before they began showing symptoms.
Of the 314 patients included in the study, 154 had tested positive for COVID-19 (defined as cases), while 160 had tested negative for COVID-19 (defined as controls). This type of study is known as a case-control study. According to an article by the CDC:
“[The odds ratio of a case-control study] quantifies the relationship between an exposure (such as eating a food or attending an event) and a disease in a case-control study. The odds ratio is calculated using the number of case-patients who did or did not have exposure to a factor (such as a particular food) and the number of controls who did or did not have the exposure. The odds ratio tells us how much higher the odds of exposure are among case-patients than among controls.”
One key observation in the study was that people who tested positive for COVID-19 were more than twice as likely as people who tested negative to have been to a restaurant in the 14 days before symptoms appeared, even though most people who tested positive for COVID-19 reported wearing a mask. COVID-19 mainly spreads by respiratory droplets that are generated through coughing, sneezing, and talking. Cloth face masks help reduce the spread of COVID-19 by minimizing the spread of respiratory droplets from an infected person.
According to the researchers, one possible explanation for this finding is that masks cannot be worn while eating or drinking, thereby diminishing their effectiveness:
“Reports of exposures in restaurants have been linked to air circulation. Direction, ventilation, and intensity of airflow might affect virus transmission, even if social distancing measures and mask use are implemented according to current guidance. Masks cannot be effectively worn while eating and drinking, whereas shopping and numerous other indoor activities do not preclude mask use.”
In summary, the claim that the study by Fisher et al. shows masks don’t work or make people sick is incorrect and based on a highly flawed comparison. Rather, the study acknowledges that effective measures for reducing the spread of COVID-19, such as face masks and physical distancing, are difficult to implement in certain situations, such as going to a restaurant, which can lead to an increased risk of infection:
“Continued assessment of various types of activities and exposures as communities, schools, and workplaces reopen is important. Exposures and activities where mask use and social distancing are difficult to maintain, including going to locations that offer on-site eating and drinking, might be important risk factors for SARS-CoV-2 infection. Implementing safe practices to reduce exposures to SARS-CoV-2 during on-site eating and drinking should be considered to protect customers, employees, and communities and slow the spread of COVID-19.”
As detailed in this review by Health Feedback, scientific evidence supports the use of face masks as an effective measure for reducing the spread of COVID-19. Health authorities acknowledge that none of the protective measures against COVID-19 spread, like handwashing, mask-wearing, and physical distancing, are 100% effective on their own. It is important for people to practice multiple protective measures to minimize risk of infection, as illustrated below by virologist Ian Mackay. However, simply because a certain measure is not 100% effective on its own is not a reason to dismiss the measure entirely (nirvana fallacy).

UPDATE (13 Nov. 2020):
On 10 November 2020, the U.S. CDC updated its recommendations on mask use, stating that cloth mask use would also help to protect the wearer, in addition to protecting others from the wearer:
“Masks are primarily intended to reduce the emission of virus-laden droplets (“source control”), which is especially relevant for asymptomatic or presymptomatic infected wearers who feel well and may be unaware of their infectiousness to others, and who are estimated to account for more than 50% of transmissions. Masks also help reduce inhalation of these droplets by the wearer (“filtration for personal protection”). The community benefit of masking for SARS-CoV-2 control is due to the combination of these effects; individual prevention benefit increases with increasing numbers of people using masks consistently and correctly.”
The “Swiss Cheese Respiratory Virus Pandemic Defense” illustration has also been updated to include more interventions, such as vaccines and cough etiquette.
REFERENCES
- 1 – Fisher et al. (2020) Community and Close Contact Exposures Associated with COVID-19 Among Symptomatic Adults ≥18 Years in 11 Outpatient Health Care Facilities — United States, July 2020. Morbidity and Mortality Weekly Report.


