Incorrect: Lockdowns are an effective public health intervention for preventing the spread of COVID-19. This measure helped to avoid the saturation of healthcare systems at the beginning of the pandemic. Face masks also reduce the spread of COVID-19, and no evidence supports claims that mask-wearing causes negative health effects when masks are correctly used.
Misleading: In combination with clinical signs presented by a patient, PCR tests can help diagnose COVID-19, as they detect the presence of the virus that causes the disease. PCR and other tests are useful for determining which public health measures must be taken to reduce the spread of COVID-19.

AFFIRMATION COMPLETE: “The survival rate of ‘Covid’ is over 99%”; “There has been NO unusual excess mortality”; “‘Covid death’ counts are artificially inflated”; “Lockdowns do not prevent the spread of disease”; “Lockdowns kill people”; “Hospitals were never unusually over-burdened”; “PCR tests were not designed to diagnose illness”; “The CT values of the PCR tests are too high”, “Masks don’t work”; “Masks are bad for your health”; “Vaccines do not confer immunity or prevent transmission”; “The vaccines were rushed and have unknown [long-term] effects”
REVIEW
On 22 September 2021, OffGuardian published an article, which was reprinted by ZeroHedge and shared by other websites like InfoWars, listing 30 claims related to COVID-19. These articles, which went viral, received altogether more than 19,000 interactions on social media platforms including Facebook and Reddit, including more than 11,000 shares, according to social media analytics tool CrowdTangle.
Although the article claimed to list “30 facts” about COVID-19, several of these “facts” are inaccurate and/or misleading, and many among them were previously debunked by Health Feedback and other fact-checkers, as we explain below. This review examines several key claims made in the articles.
Claim 1 (Inaccurate): “There has been NO unusual excess mortality”
The article presented the age-standardized mortality rate as evidence that there was no excess mortality due to the COVID-19 pandemic. In other words, that there weren’t more people dying during the pandemic compared to pre-pandemic times.
The World Health Organization (WHO) defines age-standardized mortality as “a weighted average of the age-specific mortality rates per 100 000 persons, where the weights are the proportions of persons in the corresponding age groups of the WHO standard population”.
Excess mortality associated with COVID-19 has been detected in different countries. Excess mortality is a useful estimate of the impact of the pandemic, as it reflects the increase in the number of deaths compared to the pre-pandemic period for each country, regardless of the reporting and testing of COVID-19 cases by country[1].
The WHO has warned that the numbers of deaths caused by COVID-19 may have been underestimated. According to a report published in May 2021, « at the regional level, COVID-19 excess mortality estimates range from 1.34-1.46 million in the Region of the Americas to 1.11-1.21 million in the European Region in 2020 », as shown in Figure 1.
A commentary published in March 2021 by Oxford University’s Centre for Evidence-Based Medicine reported an increase in mortality of 12.9% in the United States in 2020.
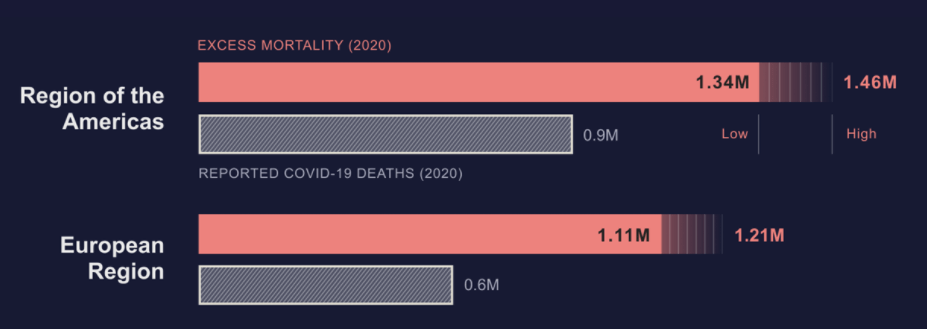
Figure 1. COVID-19 excess mortality estimates and reported deaths by WHO region, 2020. Source: World Health Organization.
This New York Times report recorded an excess of 788,900 deaths in the U.S. since the beginning of the pandemic, as well as an excess of 652,000 deaths in Russia, 600,000 in Brazil, 148,000 in Italy, 121,000 in the U.K. and 102,000 in Spain, among many other countries with excess deaths higher than the COVID-19 reported deaths.
In summary, epidemiological evidence demonstrates that the claim that “there has been no unusual excess mortality” related to the COVID-19 pandemic is false.
Claim 2 (Inaccurate): “‘Covid death’ counts are artificially inflated”
The claim that COVID-19 deaths are inflated is based on two assumptions made in the OffGuardian article: 1) that most COVID-19 cases are asymptomatic or false positives of PCR tests and 2) that people with previous comorbidities who were listed as COVID-19 deaths had actually died from the comorbidities, not COVID-19.
According to guidelines from the U.S. Centers for Disease Control and Prevention (CDC) concerning the certification of deaths due to COVID-19, “cause of death” may refer to the immediate cause of death or to the underlying cause of death. The underlying cause of death is defined as “the disease or injury which initiated the train of morbid events leading directly to death”, while the immediate cause of death is “the disease or condition that directly preceded death”.
Based on these guidelines, patients who had previous comorbidities but were listed as COVID-19 deaths had been verified to have died of COVID-19, based on the clinical chain of events leading to their deaths. A similar claim was previously debunked by Health Feedback.
And as explained above, according to the WHO, the number of deaths due to COVID-19 may be seriously underestimated rather than overestimated. Therefore, the claim that the number of COVID-19 deaths are artificially inflated contradicts existing evidence.
Claim 3 (Incorrect and Unsupported): “Lockdowns do not prevent the spread of disease”; “lockdowns are deadlier than the ‘virus’”
Lockdowns are a public health intervention which limits certain activities by the general population and private businesses, such as attending school and gatherings. Early lockdown implementation with gradual relaxation of restrictions has been shown to be an effective measure to curb COVID-19 spread [2]. This has been covered in several Health Feedback reviews here, here, and here.
The claim made in the article that lockdowns kill more people than COVID-19 is unsupported by current evidence. The benefits associated with lockdowns outweigh possible negative impacts, as this measure reduces the spread of COVID-19 and saves lives[2]. Although there were early concerns about the negative impact of the pandemic and some public health control measures on the mental health of the population[3], no evidence has been found so far of an increase in suicides or self-harm associated with the pandemic, as explained in this Insight article by Health Feedback.
Claim 4 (Inaccurate): “Hospitals were never unusually over-burdened [due to COVID-19]”
The article by OffGuardian claimed that the main argument for implementing lockdowns was to reduce the number of COVID-19 infections at the beginning of the pandemic and to avoid the saturation of healthcare systems, but asserted that “most healthcare systems were never close to collapse at all”.
The article cited Spain and Italy, where hospitals already faced a lack of beds due to flu epidemics in previous years during winter. This is correct, as was reported by Spanish news outlets in 2017 and 2018. However, the COVID-19 pandemic was even more severe than the flu epidemics, pushing the hospital systems of both countries to their limits.
In Spain, the situation in hospitals became critical due to the need for ICU beds and ventilators for COVID-19 patients who were severely ill at the beginning of the pandemic, to the point that some hospitals in Madrid refused to admit elderly patients with COVID-19, in order to have free ICU beds for younger patients with a higher chance of survival, an unprecedented event. In Italy, saturation of hospitals in the north of the country was also reported at the beginning of the pandemic.
According to this article from The Health Foundation, lockdowns prevented over-stretching of healthcare systems and reduced the number of infections and deaths from COVID-19 depending on how strict the lockdown was. Also according to the authors, while the healthcare system in the U.K. was not at full capacity during the first wave of the pandemic, measures had to be taken to prevent hospital capacity being overwhelmed.
The evidence shows that the claim that hospitals haven’t seen an unusually high number of hospitalizations isn’t true.
Claim 5 (Misleading and Inaccurate): “PCR tests were not designed to diagnose illness”; “PCR Tests have a history of being inaccurate and unreliable”; “the CT values of the PCR tests are too high”; “the majority of PCR test results are at best questionable”; “the World Health Organization (Twice) Admitted PCR tests produced false positives”
PCR stands for polymerase chain reaction. This test detects genetic material from a specific organism, like a virus. The test can detect the presence of a virus even if the infected person has no symptoms of the disease, as it has high sensitivity[4].
This fact-check by Reuters debunked a similar claim that the inventor of PCR tests stated that the tests could not be used for virus detection. As the U.S. CDC explains, PCR tests are valuable for diagnosis, as a positive test result can be used to identify a disease in a patient showing symptoms of that disease. On the other hand, a negative test in a person with symptoms can be used to rule out an active infection at the time of testing.
Contrary to what the article by OffGuardian claimed, PCR tests are highly specific, meaning that they can distinguish between patients with and without the virus[4]. This test is considered the most accurate and reliable test for detecting infection. The U.S. CDC developed diagnostic kits for COVID-19 based on the PCR test, including a Multiplex Assay that is capable of simultaneously diagnosing COVID-19 and two types of flu, caused by the influenza A and influenza B viruses.
PCR tests detect the presence of a virus by amplifying (making new copies) a small part of its genetic material. The number of amplification cycles needed to reach a threshold that can be considered a « positive » test result is known as the cycle threshold (Ct) value, which depends on the amount of virus present in a sample (viral load). Samples containing more virus require fewer amplification cycles to reach the positive threshold and therefore have a lower Ct value. The reverse is true for samples with trace amounts of virus; such samples would have a high Ct value.
As explained in this claim review by Health Feedback, a positive PCR test indicates that the person is or has been infected with the virus regardless of whether a person tested positive with a high or low viral load. The high number of COVID-19 cases detected using PCR tests is due to a large number of infected people, not due to defects in test sensitivity. Therefore, the claim that most PCR test results are questionable because Ct values are too high is false.
An information notice regarding COVID-19 PCR testing was published by the WHO in January 2021, reminding laboratory personnel to carefully interpret PCR test results when a patient’s symptoms do not match the test result. The WHO did not « admit » that the test generates false positives, as claimed in the article by OffGuardian, as explained in this review by Health Feedback.
Claim 6 (Inaccurate): “There is very little evidence supporting the alleged danger of ‘asymptomatic transmission’”
According to the WHO, both symptomatic and asymptomatic people can spread COVID-19. A study published in March 2020 found similar viral loads in asymptomatic and symptomatic COVID-19 patients, which suggested the transmission potential of asymptomatic patients[5]. Another study used meta-analysis data to develop a model assessing the impact of asymptomatic patients in the transmission of COVID-19, and found that asymptomatic cases accounted for more than half of all transmissions[6]. Therefore, the claim that there is no danger of asymptomatic transmission of COVID-19 is false.
Claim 7 (Inaccurate): “Masks don’t work”; “masks are bad for your health”
Wearing face masks has proven to be an effective public health measure in reducing the spread of COVID-19. Respiratory droplets from infected people are recognized as a mode of transmission for COVID-19. Face masks prevent respiratory droplets from being released into the air, thus reducing the spread of the disease. Multiple scientific studies, as summarized in this Scientific Brief by the U.S. CDC, have shown that mask-wearing is effective in reducing the number of infections.
There is no evidence that continued use of face masks produces negative health effects, as explained in this claim review by Health Feedback. Contrary to the claims in the article by OffGuardian, the use of face masks doesn’t increase CO2 levels in the blood, since the masks don’t prevent the passage of gases. As for the claim that the use of face masks increases the incidence of bacterial pneumonia, a fact-check by Reuters found no evidence that the use of face masks increases the risk of developing pneumonia.
Claim 8 (Incorrect): “Vaccines do not confer immunity or prevent transmission”
Immunity is defined as the ability of the body to resist a disease. COVID-19 vaccines are effective at conferring immunity, as they protect a person from severe illness and death. It has been reported that Pfizer’s COVID-19 vaccine has an 80% efficacy at preventing the disease, while Moderna’s vaccine has a 77% efficacy and Janssen’s vaccine has a 72% efficacy.
According to the U.S. CDC, vaccinated people are less likely to get the disease and less likely to transmit. Related to this, a study conducted in the U.S. found that COVID-19 vaccines from Pfizer and Moderna were effective at preventing infections, and reduced the viral load and duration of illness in re-infected people[7].
Therefore, the claim is false; vaccines confer immunity and reduce a person’s likelihood of transmitting the disease to others.
Claim 9 (Inaccurate): “Since the beginning of 2020, the Flu has ‘disappeared’”
Since the beginning of the COVID-19 pandemic, influenza cases in different countries reported to the WHO have decreased considerably, although they are still present. This decrease in cases has been related to the implementation of health measures aimed at reducing the spread of COVID-19, such as physical distancing and mask-wearing. This is because these measures also work to prevent the spread of other respiratory illnesses like the flu, as explained in this claim review by Health Feedback.
Claim 10 (Misleading): “The survival rate of “Covid” is over 99%”
The survival rate of COVID-19 is often used to downplay the public health threat posed by the disease. However, this overlooks the fact that an illness with a relatively low mortality rate can still lead to many deaths if it infects a large number of people, like COVID-19 has. This was explained in an earlier Health Feedback review. The WHO reported on 1 October 2021 that more than 233 million cases of COVID-19 were reported worldwide and more than 4.7 million people worldwide died of COVID-19.
In addition, the probability of hospitalization and death from COVID-19 aren’t uniform across the population, but vary depending on factors such as age and the presence of comorbidities[8]. Therefore, each individual’s chance of dying from COVID-19 will vary depending on their age and underlying health conditions, as explained in this fact-check by the Associated Press.
Claim 11 (Misleading and Missing context): “The vaccines were rushed and have unknown [long-term] effects”
The claim implies that corners were cut during the development of the COVID-19 vaccines, but this isn’t true. The vaccines went through all the necessary steps for vaccine development, as explained in this claim review by Health Feedback. There are several reasons why the vaccines were developed in a much shorter time compared to other vaccines. One of them is that prior knowledge of other coronaviruses and rapid sequencing of the SARS-CoV-2 genome allowed the first vaccine candidates to be developed within a few months[9]. Rapid enrollment of participants for clinical trials and overlapping of some phases of the manufacturing process also saved time, as explained in this article by Nebraska Medicine. The urgency arising from a public health crisis also led to a larger-than-usual amount of resources spent on reviewing clinical trial data submitted for vaccine authorization.
The claim that unknown long-term side effects associated with vaccines may appear in the future contradicts what we know about how vaccines work. According to Paul Goepfert, director of the Alabama Vaccine Research Clinic at the University of Alabama at Birmingham, vaccines (including mRNA vaccines) are quickly eliminated by the body, and side effects tend to show up within two months of vaccination. COVID-19 vaccines have been in use for more than a year, and to date, more than 3.59 billion people around the world have received at least one dose of COVID-19 vaccine. These observations taken together suggest that long-term side effects from the vaccines are unlikely.
Claim 12 (Inaccurate): “A ‘training exercise’ predicted the pandemic just weeks before it started”
Health emergency preparedness exercises are routinely conducted to improve response procedures and protocols for health emergencies of any kind[10].
The Johns Hopkins Center for Health Security prepared a scenario for one such exercise in 2017, based on a pandemic with SARS-like characteristics, which in the exercise was called SPARS. In addition, in 2019 the Johns Hopkins Center prepared a similar exercise, called Event 201, in partnership with the World Economic Forum and the Bill & Melinda Gates Foundation.
However, as the center clarified in a statement, they did not predict that the COVID-19 pandemic would occur shortly after the exercise, and COVID-19 does not have the same characteristics as the disease used in the exercise.
Claim 13 (Unsupported): “The majority of Covid infections are ‘asymptomatic’”
The U.S. CDC defines an asymptomatic case of COVID-19 as “an individual infected with SARS-CoV-2 who does not exhibit symptoms at any time during the course of infection”.
There is currently no consensus about the prevalence of asymptomatic COVID-19 cases. A study carried out in Henan Province, China, found that the proportion of asymptomatic cases among COVID-19 infected individuals was 42%[11]. A systematic review of 350 papers found that one-third of all reported cases were asymptomatic[12]. Another study, based on data from the U.K., found 76.5% of asymptomatic cases among 36,061 individuals with a positive test result for COVID-19[13].
Claim 14 (Misleading): “There has been a massive increase in the use of ‘unlawful’ DNRs”
The article by OffGuardian postulated that an inappropriate use of do-not resuscitate orders (DNRs) in COVID-19 patients could be the cause of excess mortality related to the pandemic. A DNR order instructs medical personnel not to do cardiopulmonary resuscitation (CPR) if a patient’s heart stops beating. But this claim contradicts OffGuardian’s first claim, which asserted that there hasn’t been “unusual excess mortality”.
As explained in this Washington Post article published early during the pandemic, the use of DNR orders, as well as other measures that may limit the amount of resources used to save a patient’s life, is intended to maximize the availability of resources in case of hospital overflow. In addition, another reason is that hospitals were concerned with protecting healthcare personnel from infection, particularly in cases when there is insufficient personal protective equipment to safely perform resuscitation on infected patients. R. Alta Charo, a bioethicist at the University of Wisconsin-Madison, explained: “It doesn’t help anybody if our doctors and nurses are felled by this virus and not able to care for us”.
A study from Sheffield University using U.S. data found that 31% of COVID-19 patients admitted to hospitals during the first wave of the pandemic had a DNR decision recorded on or before the day of admission[14]. Patients with an early DNR decision had higher mortality than other COVID-19 patients (40% versus 13%). The application of early DNR decisions was correlated with advanced age or severe comorbidities.
However, the authors also found that some patients with an early DNR decision received life-saving treatment comparable to other COVID-19 patients:
« These findings show that potentially life-saving treatments were provided to a significant proportion of people, potentially addressing concerns that [DNR] decisions may be conflated with ‘do not provide active treatment’. »
This suggests that DNRs weren’t wrongly used to increase the number of COVID-19 deaths, as the article by OffGuardian implied.
Claim 15 (Misleading): “Ventilation is NOT a treatment for respiratory viruses”; “ventilators killed people”
Mechanical ventilators serve to pump air into a person’s lungs, helping the patient breathe during a surgery or if the patient can’t breathe on their own due to a critical illness. It is true that ventilators don’t treat a respiratory infection, but they aren’t used as COVID-19 treatment in hospitals, making this a strawman argument. Instead, ventilators serve as a form of life support that helps to keep the patient alive while their body fights off illness or recovers from injury. This is particularly useful in patients with diseases that impair breathing capacity, such as COVID-19, as explained in this Yale Medicine article.
The use of mechanical ventilators involves certain risks. While it is true that mechanical ventilators can lead to pneumonia, and in some cases, damage the airway or lungs, they keep patients alive who might otherwise have severe breathing problems or are unable to breathe at all. The benefits of mechanical ventilators are considered to outweigh their risks and save lives. A similar claim was previously debunked by Health Feedback.
Claim 16 (Mostly accurate): “The vast majority of [COVID-19] deaths have serious comorbidities”
Certain medical conditions, such as cancer, cardiovascular disease, obesity or diabetes, have been linked to increased chances of developing severe COVID-19. A literature review of studies that recorded COVID-19 deaths at the onset of the pandemic found the presence of one or more comorbidities in 84.1% of cases, with significant mortality rates related to cardiovascular disease (related to 34.9% of recorded deaths), hypertension (35.2%), and diabetes (33.2%)[15].
Claim 17 (Mostly accurate): “Average age of ‘Covid death’ is greater than the average life expectancy”
Age is a determining factor in hospitalizations and deaths due to COVID-19. The majority of COVID-19 deaths in the U.S. have been observed in people older than 75 years, as shown by data from the U.S. CDC. The average life expectancy in the U.S. is 79 years, according to data from the real-time statistics website Worldometer.
The situation is mirrored in other countries, with the average age at which people die being 80 years in Italy (life expectancy of 84), 82 in the U.K. (life expectancy of 82) and 86 in Spain (life expectancy of 84). In Canada, the majority of COVID-19 deaths were over 80 years old, while the average life expectancy is 83. Therefore, the average age of people who died of COVID-19 in these countries is indeed close to or above average life expectancy.
Context for statements that were not precise enough to be verified
Because certain statements made in the OffGuardian article lacked sufficient detail and/or a clear definition of the terms used, we didn’t consider these statements to be verifiable. But in light of their potential to mislead readers, we decided to provide additional context regarding these statements.
1. “Covid mortality exactly mirrors the natural mortality curve”
Both the risk of dying from COVID-19 and the background risk of dying increase with age, as explained in this article from the Winton Center for Risk Communication and Evidence. However, as the author pointed out, COVID-19 increases the background probability of dying.
2. “The scientific basis for Covid tests is questionable”
Several types of tests can be used for the detection of SARS-CoV-2. As explained above, the PCR test detects a specific genetic sequence of the virus SARS-CoV-2. On the other hand, antigen tests detect SARS-CoV-2 viral proteins (antigens). Both antigen and PCR tests are performed on mucosal samples taken with a swab. A third type of test is the antibody or serology test, which detects from a blood sample the response that the body has generated after contact with SARS-CoV-2 (antibodies).
Different kinds of tests are useful to assess the epidemiological situation, and to determine which public health measures must be taken to curb the spread of the disease. The WHO indicates that diagnostic testing for SARS-CoV-2 is an important component of COVID-19 control and prevention strategies.
3. “Masks are bad for the planet”
Face masks, like other man-made waste, can indeed cause problems if they are incorrectly disposed of. The article by OffGuardian cited a study from Swansea University, in which researchers found that face masks released plastic microfibers and heavy metals when submerged in water[16]. Shifting from disposable to reusable face masks has been suggested as a way to minimize their potential negative impact on the environment. However, these environmental problems are linked to inadequate waste treatment, and face masks are not inherently “bad for the planet”, as claimed.
4. “Covid ‘vaccines’ are totally unprecedented”
Prior to the development of COVID-19 vaccines, no other vaccine against a coronavirus had been developed. The reasons for the rapid development of COVID-19 vaccines have been new scientific advances, especially those related to RNA and its delivery to cells; previous work on other coronaviruses, like those that caused the SARS and MERS outbreaks; and the large amount of resources devoted to vaccine development, as explained in this article by Science News.
5. “Vaccine manufacturers have been granted legal indemnity should they cause harm”
In the U.S., the Public Readiness and Emergency Preparedness Act, known as PREP Act, has been invoked to exclude companies that manufacture products needed during a health emergency from potential claims, as reported by the CNBC. This protection should be in place until at least 2024.
As for the EU, liability terms varied between contracts with different vaccine manufacturers, as reported for Pfizer and AstraZeneca. Member of the European Parliament Liudas Mažylis registered a parliamentary question regarding possible compensation for side effects of COVID-19 vaccines, which was answered by the European Commission stating that “communication about compensation procedures for side effects should take place at national level”.
6. “The EU was preparing ‘vaccine passports’ at least a year before the pandemic began”
The European Centre for Disease Prevention and Control produced a series of reports (see here and here) in 2018 analyzing the status of various immunization programs against communicable diseases in the EU. Part of these reports identified problems associated with vaccine hesitancy, defined in the reports as a delay in accepting or refusing to participate in immunization programs despite the availability of a vaccine.
The European Commission also produced a roadmap detailing the steps to be taken to improve immunization against various infectious diseases in the EU, including the proposal for a “common vaccination card/passport for EU citizens”, to be undertaken in 2022. The European Commission reports were published in 2018, so they are unrelated to the COVID-19 pandemic, contrary to what the article by OffGuardian implied.
REFERENCES
- 1 – Beaney et al. (2020) Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? Journal of the Royal Society of Medicine.
- 2 – Mégarbane et al. (2021) Is Lockdown Effective in Limiting SARS-CoV-2 Epidemic Progression?—a Cross-Country Comparative Evaluation Using Epidemiokinetic Tools. Journal of General Internal Medicine.
- 3 – Gunnell et al. (2020) Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry.
- 4 – Kortela et al. (2021) Real-life clinical sensitivity of SARS-CoV-2 RT-PCR test in symptomatic patients. PLoS One.
- 5 – Lirong et al. (2020) SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. The New England Journal of Medicine.
- 6 – Johansson et al. (2021) SARS-CoV-2 Transmission From People Without COVID-19 Symptoms. Journal of the American Medical Association.
- 7 – Thompson et al. (2021). Prevention and Attenuation of Covid-19 with the BNT162b2 and mRNA-1273 Vaccines. The New England Journal of Medicine.
- 8 – Mason et al. (2021) Age-Adjusted Associations Between Comorbidity and Outcomes of COVID-19: A Review of the Evidence From the Early Stages of the Pandemic. Frontiers in Public Health.
- 9 – Wu et al. (2020) A new coronavirus associated with human respiratory disease in China. Nature
- 10 – Skryabina et al. (2017) What is the value of health emergency preparedness exercises? A scoping review study. International Journal of Disaster Risk Reduction.
- 11 – Li et al. (2021) Estimating the Prevalence of Asymptomatic COVID-19 Cases and Their Contribution in Transmission – Using Henan Province, China, as an Example. Frontiers in Medicine.
- 12 – Sah et al. (2021) Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis. Proceedings of the National Academy of Sciences.
- 13 – Petersen and Phillips (2020) Three Quarters of People with SARS-CoV-2 Infection are Asymptomatic: Analysis of English Household Survey Data. Clinical Epidemiology.
- 14 – Sutton et al. (2021) Do not attempt cardiopulmonary resuscitation (DNACPR) decisions in people admitted with suspected COVID-19: Secondary analysis of the PRIEST observational cohort study. Resuscitation.
- 15 – Bajgain et al. (2021) Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. American Journal of Infection Control.
- 16 – Sullivan et al. (2021) An investigation into the leaching of micro and nano particles and chemical pollutants from disposable face masks – linked to the COVID-19 pandemic. Water Research.



