RECLAMACION: “Vaccine herd immunity doesn’t exist [...] and here’s why: 1. Because 100 percent of the population would have to be vaccinated for that to work. 2. Vaccines would have to promise immunity and they don’t. […] 3. Immunity from vaccines is temporary […] 4. Live virus vaccines shed. […]
REVIEW
As COVID-19 vaccination campaigns move forward in a number of countries, journalists, healthcare professionals and scientists have raised the questions of when a country can expect to reach herd immunity and if they are close to reaching it.
Herd immunity is a concept that describes the point at which the population as a whole is protected from an infectious disease. This point occurs when enough people in a population or “herd” are protected from that disease, either through vaccination or through previous infection. This in turn protects even individuals susceptible to the disease, because they are a member of a “herd” where the majority are protected, making it unlikely for the susceptible individual to become infected.
To better understand the concept of herd immunity, picture 100 people in a room. When a new infectious disease appears, everyone is susceptible to the disease and each person, once infected, has the potential to spread that disease to their neighbors. However, if a large percentage of the population is immune, even if the disease infects one of the few susceptible individuals, the pathogen will have a hard time spreading because the majority is protected. When this is achieved, the population is considered to have herd immunity.
In an Instagram post published on 24 April 2021, Laura Elizabeth claimed that herd immunity from vaccines doesn’t exist and provided four explanations for her claim. The post received over 7,000 likes and 200 comments as of 30 April 2021. As we demonstrate below, this claim is inaccurate, as are all four explanations given by Elizabeth.
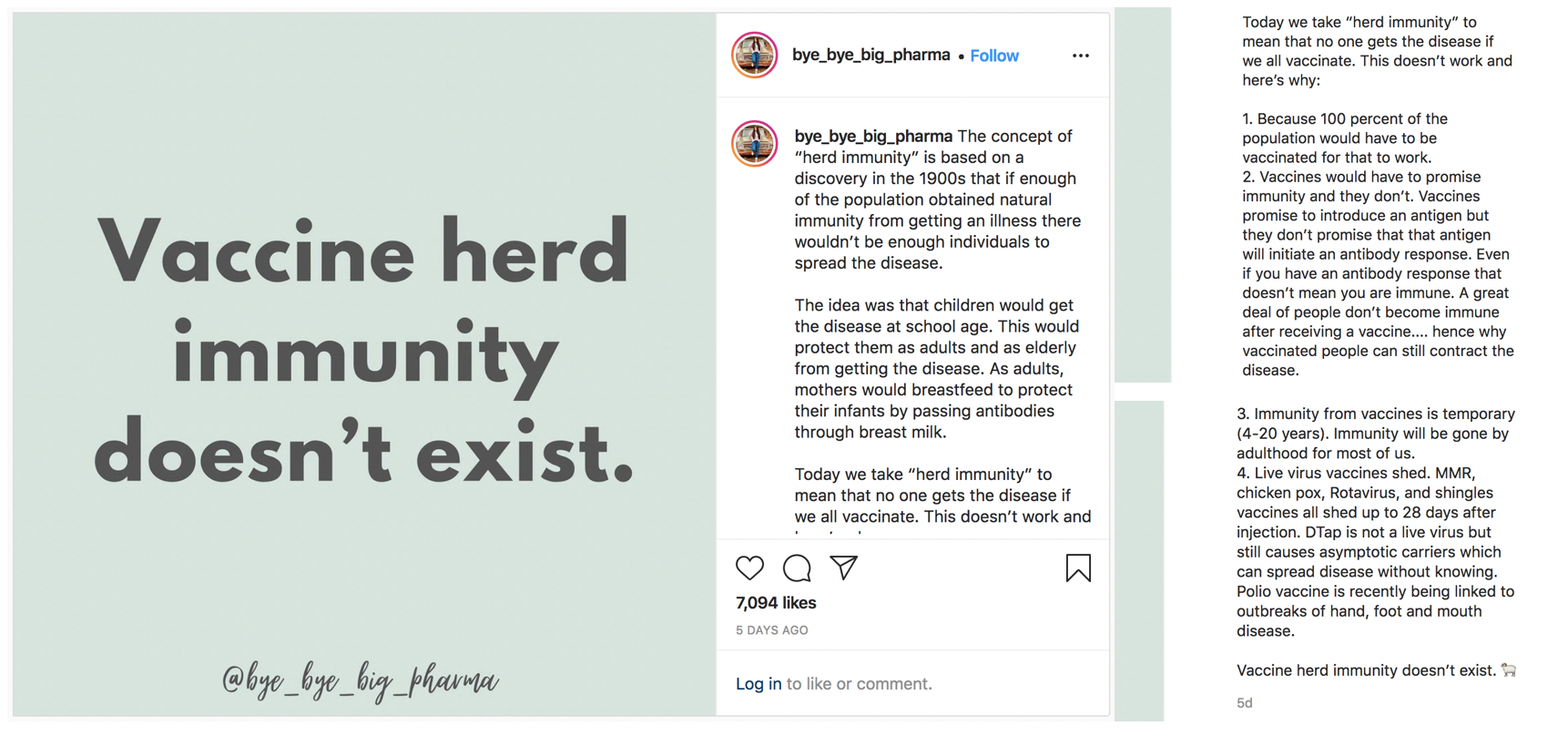
Figure – Screenshot of Laura Elizabeth’s post about vaccine herd immunity. On the left is her claim, and on the right are the four inaccurate reasons to explain her claim.
What percentage of the population needs to be vaccinated to achieve herd immunity varies for each infectious disease
Elizabeth claimed that “100 percent of the population would have to be vaccinated” to achieve herd immunity. However, in several cases, herd immunity can be achieved even when less than 100% of the population is vaccinated. “The more infectious a disease is, the higher the proportion of the population that has to be protected before we get to herd immunity,” explained epidemiologist Gypsyamber D’Souza, a professor at the Johns Hopkins Bloomberg School of Public Health, in a video released by Johns Hopkins.
For a highly infectious disease like measles, where each infected person on average transmits the virus to between 12 to 18 other individuals, at least 95% of the population must be vaccinated to achieve herd immunity. For a less infectious disease like polio, the necessary threshold of vaccinated individuals is about 80%. The vaccine threshold for COVID-19 is still a matter of debate, but recent estimates range from 70 to 90 percent.
In short, herd immunity requires that a sufficiently high percentage of the population be protected, so that it is difficult for the infectious disease to spread through the population. But that percentage varies greatly depending on the characteristics of the disease, especially how infectious it is. Hence, Elizabeth’s claim that “100 percent of the population would have to be vaccinated” for herd immunity to be achieved is inaccurate.
Vaccines provide the immune system with a weakened or inactive “sneak peek” of a pathogen, allowing it to generate immunity in a safe manner
The immune system is a “complex network of cells, tissues, organs, and the substances they make that helps the body fight infections and other diseases,” according to the U.S. National Cancer Institute. When a person’s immune system recognizes an invading pathogen for the first time, the system begins to address the problem. White blood cells converge on the site of the infection, while antibodies that specifically target that pathogen are produced. It can take several days for antibodies to develop and, in the meantime, the infected individual may become ill. Following this first exposure, however, the immune system will remember this pathogen and more quickly mount an immune response when it encounters the pathogen again.
Vaccines work by providing a person’s immune system with a sneak peek of a pathogen. This sneak peek involves a weakened or inactive part of the pathogen, which allows the vaccinated person’s immune system to create antibodies against the pathogen and avoid the risks of an actual infection. When an individual is exposed to a pathogen they’re vaccinated for, their immune system can quickly respond to it.
In her Instagram post, Elizabeth claimed that vaccines don’t promise immunity. That is inaccurate. Immunity is the ability of the body to resist a particular disease, and that is exactly what vaccines are designed to provide. By giving a sneak peek of a pathogen, vaccines allow an individual to swiftly mount an immune response when they encounter the pathogen in the future.
Elizabeth also inaccurately claims that “a great deal of people don’t become immune after getting the vaccine.” No vaccine is 100% effective, which is why some individuals may still get infected after they’ve been vaccinated. But the percentage of individuals who do not generate immunity following vaccination is small. For instance, about one percent of people who receive both doses of the Measles, Mumps, Rubella (MMR) vaccine don’t develop protective immunity.
Both natural and vaccine immunity can wane depending on the pathogen. This is why booster shots are provided for certain vaccines
In her post, Elizabeth claimed that immunity from vaccines is temporary. This is inaccurate because the duration of immunity generated by both vaccines and natural infection varies for different pathogens. For instance, people who receive two doses of the MMR vaccine are considered to have lifelong immunity for both measles and rubella. However, immunity to mumps decreases over time, which is why the CDC recommends a booster shot of the MMR vaccine during mumps outbreaks. In general, vaccine boosters are recommended because of waning immunity.
Elizabeth also implied that natural immunity is lifelong and therefore superior to vaccine immunity. This isn’t the case, because infection with the pathogen can generate a dramatic range of immune responses. In the case of COVID-19, for instance, as many as 9% of recovered people have no detectable antibodies, although many who survive the disease develop immunity that may persist for years. Furthermore, those with a mild illness from COVID-19 may see their immunity wane after a few months.
One possible reason for individual variation in immunity following infection is that individuals are exposed to different amounts of the virus. With vaccines, however, everyone receives a similar dose that is known to be effective at generating an immune response. In a piece for The Conversation, immunologist Jennifer Grier, an assistant professor at the University of South Carolina, explained that “COVID–19 vaccines offer safer and more reliable immunity than natural infection,” because immunity following natural infection can be unpredictable. As detailed in a previous Health Feedback review, vaccines also allow individuals to gain immunity without the risks associated with natural infection.
There are many vaccine design strategies and most vaccine types do not cause “virus shedding,” which is extremely rare
There are a few vaccine technologies that are commonly used. The classical types are inactivated, live-attenuated, and subunit vaccine designs. With the COVID-19 vaccines, two new designs have been added to the repertoire: mRNA and viral vector vaccines.
Inactivated vaccines use a killed version of the pathogen to confer immunity. Examples of inactivated vaccines include the flu, polio, Hepatitis A and rabies vaccines. Live-attenuated vaccines use an attenuated or weakened version of the pathogen, which is unable to cause disease, to generate immunity. Examples of live-attenuated vaccines include the MMR, rotavirus, smallpox, chickenpox and yellow fever vaccines.
Subunit vaccines use only a component from the pathogen, like a protein, to confer immunity. The Hepatitis B, human papillomavirus, whooping cough, pneumococcal, meningococcal, and shingles vaccines are examples of subunit vaccines.
Among the COVID-19 vaccines are mRNA and viral vector vaccines, two designs that deliver information to cells on how to produce a pathogen’s protein. These proteins then trigger the immune response, generating immunity.
In her post, Elizabeth claimed that “all live virus vaccines shed.” Vaccine shedding is the idea that vaccinated individuals will release or “shed” viruses into the population. Because most vaccine design strategies use a killed pathogen or only part of a pathogen, none of these types of vaccines can lead to vaccine shedding. In her post, Elizabeth writes that the shingles vaccine sheds, however, the shingles vaccine is a subunit vaccine and can’t cause vaccine shedding.
Because they contain a weakened version of the pathogen, live-attenuated vaccines have the potential to shed live viruses. However, what’s being shed is the weakened version of the pathogen used in the vaccine, which doesn’t make people sick. One example of a vaccine that causes shedding is the smallpox vaccine, which helped eradicate the disease and is no longer routinely administered. For this vaccine, shedding could happen at the site of injection up to 19 days. The oral poliovirus (OPV) vaccine also leads to shedding of the weakened poliovirus in up to 90% of infants [1]. Some countries have swapped the OPV for the inactivated poliovirus (IPV) vaccine, which doesn’t shed, because in rare occasions the shed vaccine virus may mutate and cause polio.
Of the routine vaccines given, both the rotavirus and chickenpox vaccines do shed, but in both cases infection is unlikely. For rotavirus, the vaccinevirus is shed in the stool and proper hygiene, such as hand washing, can prevent infection. In the case of the chickenpox vaccine, some people develop a rash after vaccination and the vaccine virus can shed from the rash. If this happens, individuals who aren’t immunocompetent or not yet vaccinated should stay away from the vaccinated individual until the rash is gone.
As such, though live virus vaccines can shed, the risk of infecting others is low because it’s the weakened version of the virus that is shed and individuals can take additional precautions to prevent infection. As such, Elizabeth’s claim that “all live virus vaccines shed” is misleading because it doesn’t provide a complete picture of vaccine shedding. Particularly, it fails to mention that what is shed is the weakened version of the virus.
Conclusion
Herd immunity is achieved when the majority of a population is immune to a pathogen; this makes it hard for the pathogen to circulate in the population, which indirectly provides protection to the minority of individuals who aren’t immune. The safest way to achieve herd immunity is to vaccinate a very large percentage of the population. The World Health Organization has spoken against strategies that aim to achieve herd immunity through natural infection, since “this would result in unnecessary cases and deaths”. Therefore, claims that vaccines don’t provide immunity and therefore cannot lead to herd immunity are inaccurate.
REFERENCES
- 1 – Holubar et al. (2017) Shedding of Oral Poliovirus Vaccine (OPV) by HIVInfected and -Uninfected Mothers of OPV-Vaccinated Zimbabwean Infants. Journal of the Pediatric Infectious Diseases Society.